by admin
Share

The Problem With Traditional Primary Care Today:
In the realm of healthcare, primary care stands as the cornerstone of a functional system, acting as the frontline defense for individuals seeking medical attention. However, despite its critical role, primary care faces numerous challenges that hinder its effectiveness and accessibility. From rural regions struggling with provider shortages to systemic issues like fragmentation of care and emphasis on acute care over preventative care, these challenges demand attention and innovative solutions to ensure equitable access and quality care for all.
Access and Availability:
One of the most pressing issues in primary care is the lack of accessibility, particularly in underserved regions. Rural areas, in particular, often suffer from a shortage of primary care providers, resulting in long wait times for appointments and difficulty accessing necessary care. This disparity in access can exacerbate existing health inequalities, leaving vulnerable populations without essential medical services.
Fragmentation of Care:
Another significant challenge is the fragmentation of care within the healthcare system. Fragmentation occurs when there is a lack of coordination among different healthcare providers and services, leading to inefficiencies, duplication of tests, and ultimately, gaps in patient care. This disjointed approach not only undermines the quality of care but also increases healthcare costs and administrative burdens.
Emphasis on Acute Care vs. Preventive Care:
Within healthcare systems, there is often a disproportionate emphasis on acute care over preventive care. While acute care addresses immediate health concerns, preventive care plays a crucial role in early intervention and disease prevention. Neglecting preventive measures not only undermines long-term health outcomes but also places added strain on healthcare resources.
Addressing the Challenges with Primary Care:
Addressing these challenges requires a multifaceted approach that involves collaboration among policymakers, healthcare providers, payers, and community stakeholders. Strategies may include incentivizing primary care in underserved areas, promoting care coordination through technology and team-based approaches, investing in physician well-being and resilience programs, shifting towards value-based care models that prioritize preventive services, and implementing policies aimed at reducing health disparities.
That is why Delphi Enhanced Primary Care is dedicated to delivering excellence in primary care through accessible, affordable pricing. By prioritizing patient-centered care and leveraging innovative approaches, such as telemedicine and care coordination, Delphi Enhanced Primary Care aims to overcome barriers to access and provide comprehensive, high-quality healthcare services to individuals and communities in need.
In conclusion, while primary care faces numerous challenges, there are opportunities for improvement and innovation to ensure equitable access and high-quality care for all individuals. By addressing issues related to access, coordination, time constraints, burnout, preventive care, financial pressures, and health disparities, we can build a stronger, more resilient primary care system that meets the needs of diverse populations and promotes better health outcomes for everyone.
A huge congratulations to Jeffrey Calegari. DO, FACP for being recognized on Castle Connolly’s 2025 Top Doctors List! Castle Connolly Top Doctors are peer-nominated, and thoroughly vetted by a physician-led research team. The Top Doctor nominees represent the top 7% of all U.S. practicing physicians. These doctors are best-in-class healthcare providers, embodying excellence in clinical
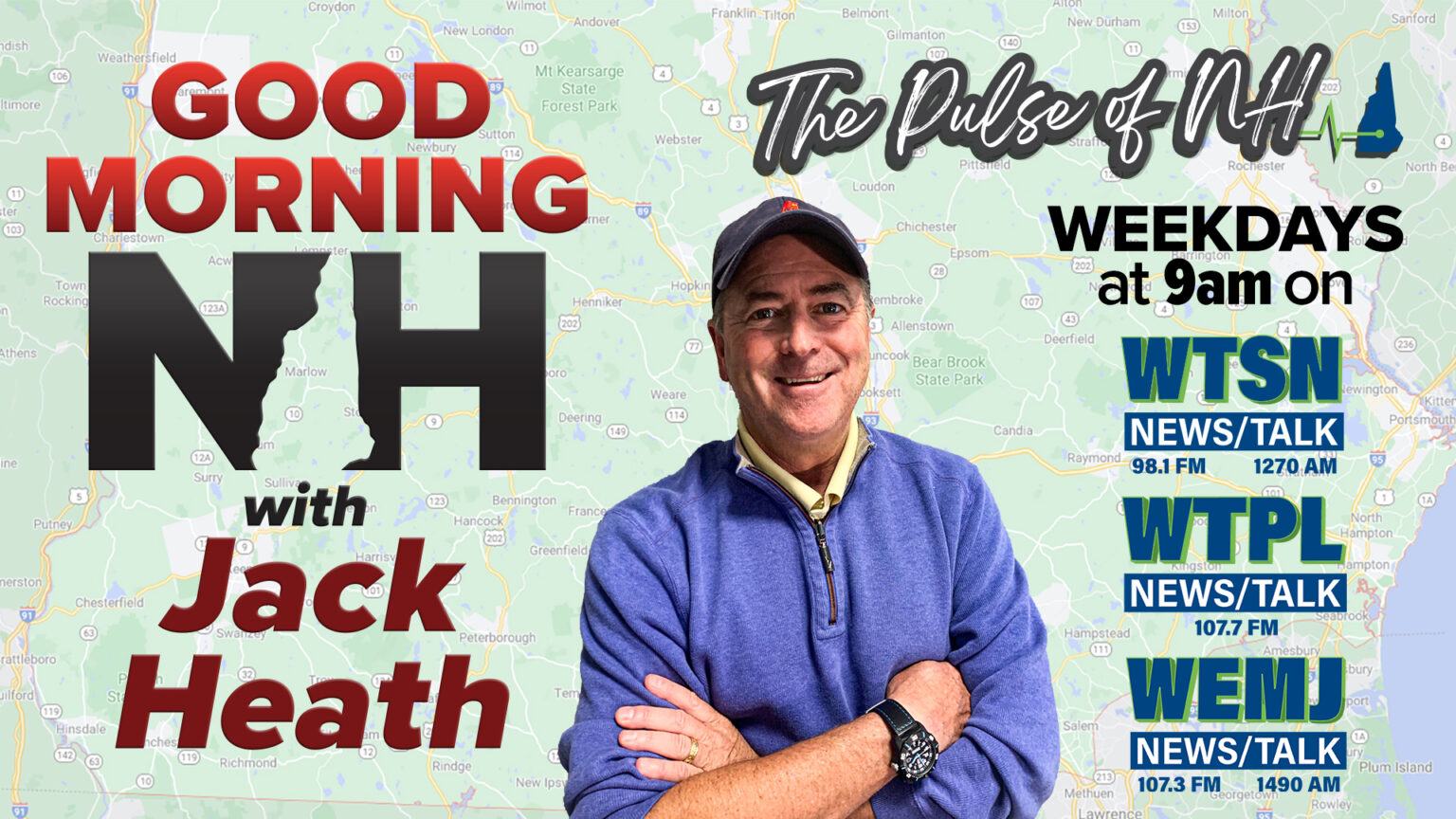
Andy Vailas of Delphi Healthcare is in the WFEA studio with Dr. Jeff Calegari and Dr. Jennifer Fishbein to discuss the personal approach patients should expect from their healthcare provider and the one-on-one relationships that are the foundation of Delphi Enhanced Primary Care.